A massive 7.5 million people were diagnosed with tuberculosis in 2022, the highest number ever – but this is positive as it indicates that countries’ ability to detect the disease is recovering after the COVID-19 pandemic, according to the World Health Organization (WHO) 2023 Global tuberculosis (TB) report.
The two countries that contributed most to the global rebound in new diagnoses were India and Indonesia, together accounting for 56% of the increase between 2021 and 2022. They were followed by Philippines (11% of the global increase) and Pakistan (8.4%).
Meanwhile, an estimated 10.6 million people fell ill with TB in 2022 – 300,000 more than the previous year, with WHO’s South-East Asia Region (46%), Africa (23%) and the Western Pacific (18%) worst affected.
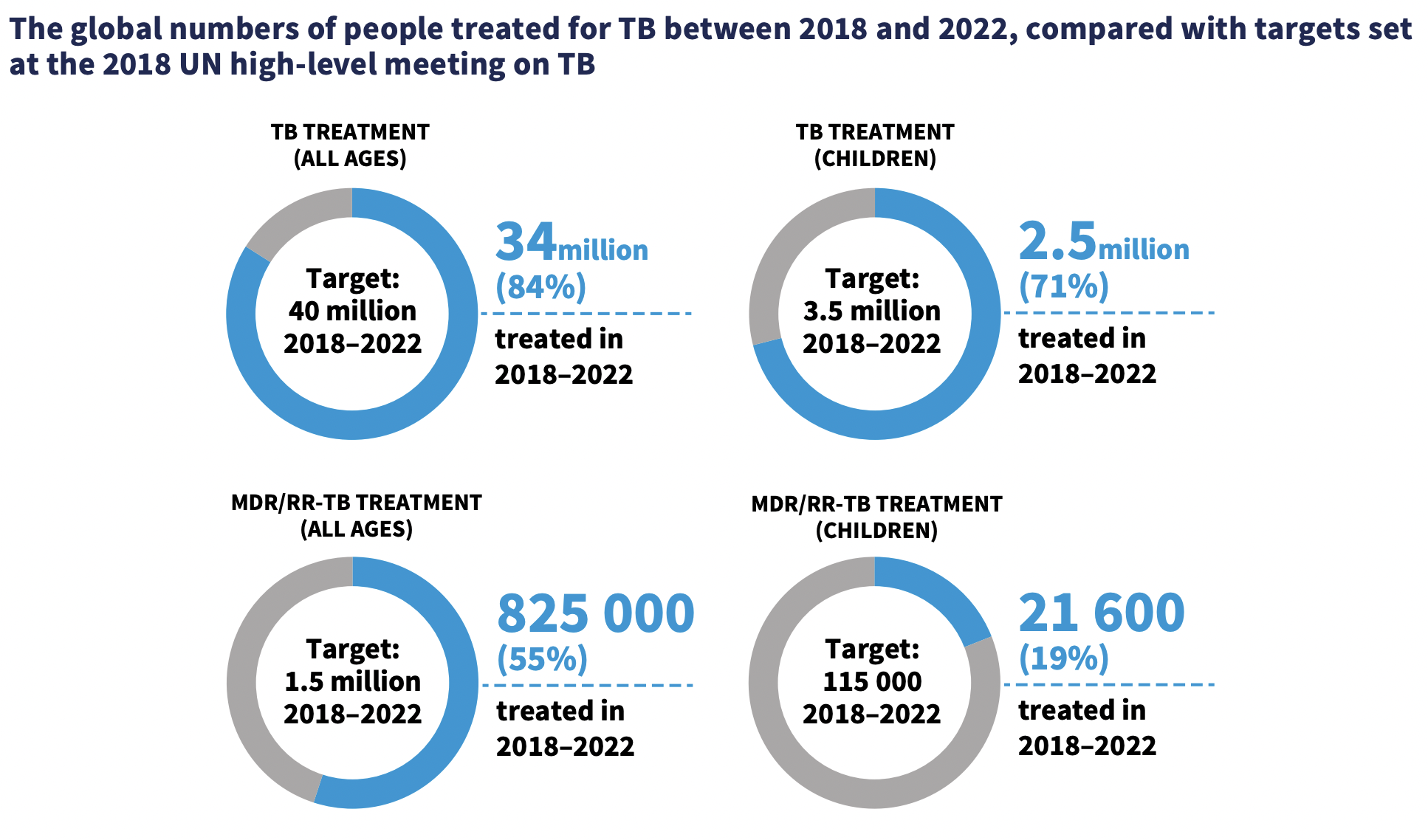
But the good news for those with TB is that treatment coverage has recovered to the pre-pandemic level of 70%, up from 62% in 2021.
Slight decrease in deaths

TB was the second leading cause of death in 2022, beaten only by COVID-19 – despite being “completely preventable and curable”, said Dr Tereza Kasaeva, WHO’s Global TB Programme director, at the report’s launch on Tuesday.
“What is missing? Prioritisation and enough investment, as we have much better tools for successful treatment, even for the most severe forms of drug-resistant TB.”
However, TB deaths were down to an estimated 1.3 million, in comparison to an estimated 1.4 million for 2020 and 2021, according to the report.
But the net reduction in deaths between 2015 to 2022 is only 19% – far from the WHO End TB Strategy milestone of a 75% reduction by 2025.
The WHO African and European regions have made the best progress in cutting deaths since 2015, while 47 countries have achieved reductions of at least 35%
Drug-resistant TB is a ‘public health crisis’
“Multidrug-resistant TB remains a public health crisis,” said Kasaeva, adding that only two out of five people with multidrug-resistant or rifampicin-resistant TB (MDR/RR-TB) received treatment last year.
With around 410,000 people developing drug-resistant TB in 2022, Kasaeva described drug-resistant TB as “stable” with “no quite clear progress toward the decrease of the burden”.
“The cumulative reduction in the TB incidence rate from 2015 to 2022 was only 8.7%, far from the WHO and TB strategy milestone over 50% reduction by 2025.”
Some 42% of the global burden of people with drug-resistant TB comes from just three countries – India (27%), the Philippines (7.5%) and Russia (7.5%).
“The uptake of the latest recommendations of the WHO for the shorter treatment option is not not fast enough,” said Kasaeva. “That’s why we can’t say that we cannot celebrate any, any progress. It’s stable is concerning and a remain should be improved significantly.
On the positive side, almost three-quarters (73%) of people diagnosed with pulmonary TB were tested for rifampicin resistance, up from 69% in 2021. Some 4.4% were diagnosed with MDR/RR-TB.
The cumulative number of people with MDR/RR-TB on treatment from 2018 to 2022 was 825 000 – 55% of the 5-year target of 1.5 million. For children, the cumulative number was 21 600 – a dismal 19% of the 5-year target of 115 000.
But the report notes that there have been “steady improvements in the treatment success rate for people diagnosed with MDR/ RR-TB”, although its most latest figures are from 2020, when the treatment success rate was 63%.
“By the end of 2022, 40 countries had started to use the new six-month BPaLM/BPaL regimen to treat people with MDR/RR-TB or pre-XDR-TB. A total of 92 countries were using the shorter nine-month oral regimens for the treatment of MDR/RR-TB,” the report notes.
Price reductions
However, Medecins sans Frontieres (MSF) notes that price reductions for the TB test GeneXpert MTB/RIF Ultrakey to diagnose TB, and the drug bedaquilinean essential part of the new shorter and safer DR-TB treatment regimens, has made the scale-up of these medical tools “significantly more achievable”.
In September, US corporation Cepheid reduced the price of the GeneXpert MTB/RIF Ultra test in high-TB-burden countries by 20% (from US$9.98 to $7.97).
Meanwhile, Johnson & Johnson decided not to enforce its secondary patents for bedaquiline in 134 low-and middle-income countries. J&J also granted Stop TB Partnership´s Global Drug Facility`s (GDF) a license that enabled it to tender, procure, and supply generic versions of bedaquiline to most LMICs.
The WHO first recommended the GeneXpert MTB/RIF as the initial test to diagnose TB in December 2010and the shorter, safer and more effective all-oral six-month DR-TB treatment regimens BPaLM and BPaL in December 2022.
“Although today’s TB statistics once again highlight how TB, a neglected but curable disease, keeps killing millions of people year after year, there may be light on the horizon,” said Dr Gabriella Ferlazzo, TB Medical Adviser of MSF’s Access Campaign.
“Over the last three months, we’ve witnessed a striking string of good news for TB, with long-fought price reductions finally coming through for better tests and drugs, and governments meeting at the UN [at the high-level meeting on TB in September] to promise to ramp up TB testing, treatment and prevention for their people, including children.”
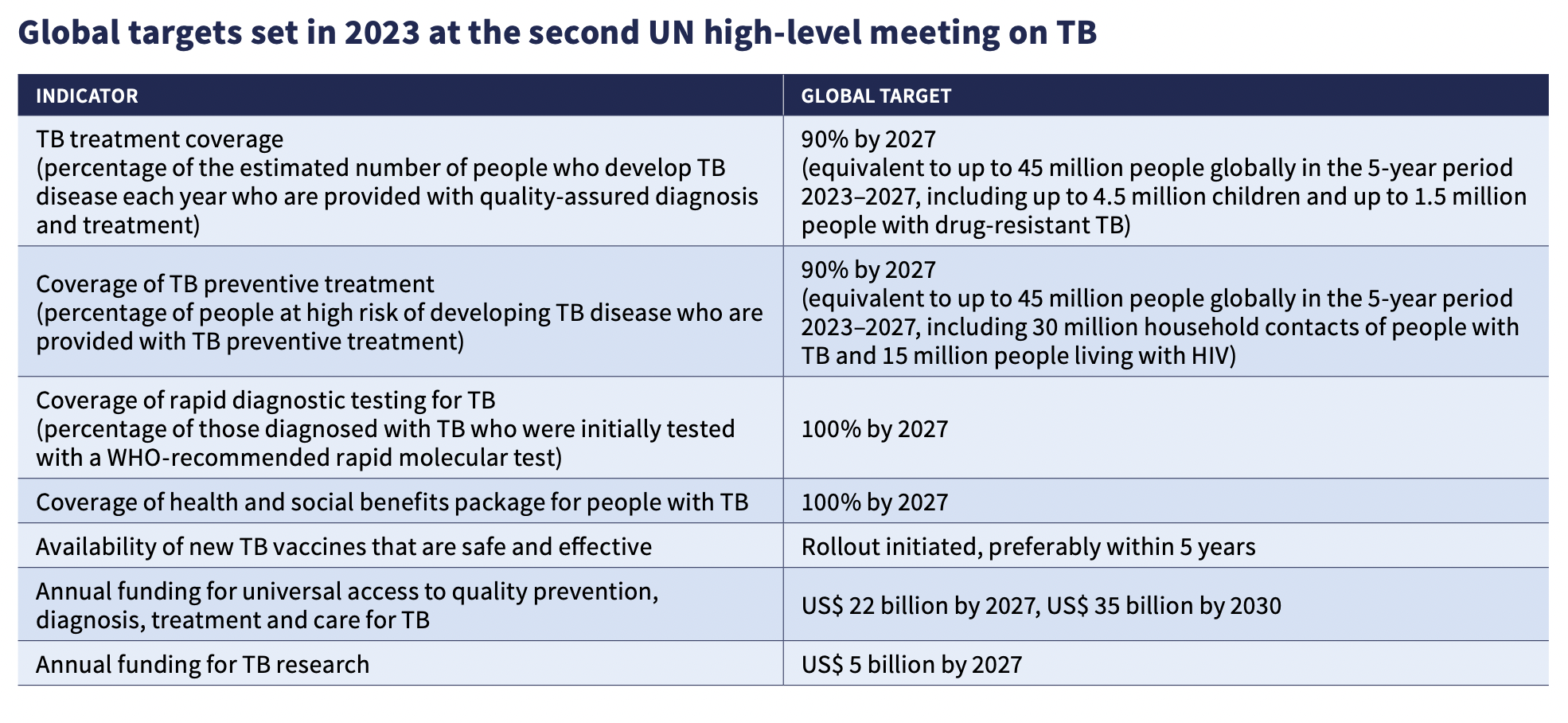
The UN High-Level Meeting on TB set new targets for 2023-2027, including reaching 90% of people in need with TB prevention and care services, using a WHO-recommended rapid test as the first method of diagnosing TB, providing a health and social benefit package to all people with TB, ensuring the availability of at least one new TB vaccine and closing funding gaps for TB implementation and research by 2027.
Ferlazzo called on governments to “use the WHO-recommended tools and strategies we now have to diagnose and treat everyone who needs it, and to increase funding for TB research and care.”
Stop TB Partnership Executive Director, Lucica Ditiu, paid tribute to all those who had managed to diagnose and treat the 7.5 million people with TB.
“Now that we have shown what can be done – can we get the financial resources and the political commitment so that we are done once and for all with this disease? It is a matter of choice for the governments, donors, and all of us,” she added.
‘Catastrophic’ out-of-pocket costs

However, the report also notes that more than half of TB patients and their households face “catastrophic health costs” – medical expenses as well as indirect costs, such as travel expenses to pick up their daily medicines, income loss, food supplements and the cost of carers.
“These costs amount to greater than 20% of total household income,” said Handaa Enkh-Amgalan, a TB survivor from Mongolia.
“Twelve years ago, I was one of those statistics where my family and I were affected by the same level of financial burden of TB that we are seeing in this report. My mom and I faced a tough choice to make. It was down to either affording bread for me and my siblings or going to a TB clinic to have an X-ray done for diagnosis,” said Enkh-Amgalan.
“My mom was able to make the decision to head to a clinic. But there are many more people who are simply unable to make that decision. TB patients are often labelled and stigmatised as irresponsible or non-compliant. These catastrophic costs and stigma are two of the many barriers that are driving millions of patients away from seeking diagnosis and treatment.”
Lack of funds
“Less than half of the $13 billion needed for TB prevention, diagnosis, treatment and care to achieve the global targets was mobilised,” said Kasaeva.
Around 80% of spending on TB services in 2022 came from domestic sources, yet “for low and middle income countries, international donor funding remains crucial”, she added.
The US contributes about 51% of international donor funding for TB and Cheri Vincent, TB Division Chief at the US Agency for International Development (USAID), stressed her government’s “deepest commitment” to move forward on the UN targets.
Image Credits: Stop TB Partnership.
Combat the infodemic in health information and support health policy reporting from the global South. Our growing network of journalists in Africa, Asia, Geneva and New York connect the dots between regional realities and the big global debates, with evidence-based, open access news and analysis. To make a personal or organisational contribution click here on PayPal.