As the rate of cesarean sections continues to rise, it’s essential to understand the reasons behind this trend and the potential risks and benefits associated with the procedure. Dr. Preethi Prabhakar Shetty, Obstetrician and Gynaecologist at Apollo Hospitals, Bengaluru, shares valuable insights on C-sections, from the indications and complications to long-term health implications and recovery.
Excerpts
Why has WHO moved away from setting an ideal C-section rate?
The World Health Organization (WHO), doesn’t believe in setting an ideal C-section rate anymore. Earlier, it was 15%, but now they say every woman who needs a Cesarean should receive it. With people having pregnancies later, medical complications, and fertility issues on the rise, the need for C-sections will vary. The focus is on ensuring women who need it get the procedure, rather than adhering to a specific rate.
Under what circumstances is a cesarean section typically recommended?
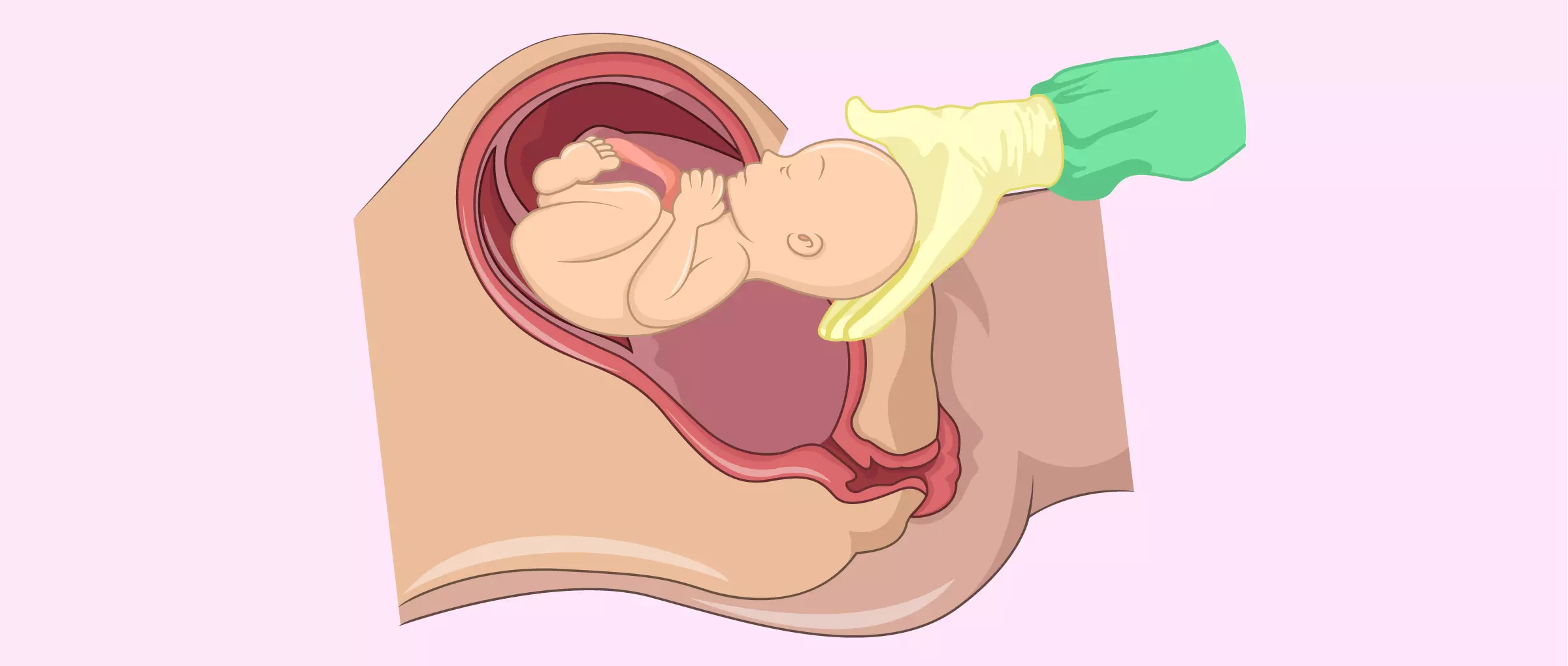
A C-section is performed when the vaginal route is risky for the mother or baby. Indications include fetal distress, obstructed or prolonged labor, Cephalopelvic disproportion (CPD), malpresentations, and placental abnormalities like placenta previa or abruption. These conditions make a surgical delivery through the abdominal route necessary for a safe outcome
Can you explain the various risks and complications that can arise from a C-section?
C-sections carry several risks, including anesthesia complications, intra-op injuries to surrounding structures, hemorrhage, infection, and blood clots. Long-term complications include adhesions, placenta accreta, and scar rupture in future pregnancies. Even babies born via C-section may face issues like tachypnea, accidental injury, and potentially higher risks of allergies and asthma. It’s crucial to weigh the pros and cons and make an informed decision that’s best for both mother and baby.
How often do complications occur in C-sections
The risk of complications in C-sections is around 1-3%, which isn’t very high, but it’s crucial to inform patients about these risks. With more patients opting for C-sections at their request, it’s essential to discuss the complications and recovery period thoroughly before proceeding.
What are the benefits of a planned C-section compared to an emergency C-section
A planned C-section is less stressful and allows the medical team as well as the pregnant woman to be fully prepared for potential complications. In high-risk cases like placenta previa, planning ahead is crucial. In contrast, emergency C-sections can be more challenging due to the urgency and potential lack of preparedness. While planning is beneficial, not all situations can be anticipated, and emergencies will always arise.
What is the typical recovery time after a C-section, and what precautions or measures should be taken to ensure a smooth recovery?
After a C-section, the hospital stay is typically three days, and total recovery takes six to eight weeks. Immediate recovery is around a week. It’s a myth that C-section patients need complete bed rest—In fact, we encourage ambulation to prevent complications like blood clots and embolic phenomenon. Early movement helps prevent these risks.
Can a woman who had a previous C-section opt for a vaginal birth in her next delivery
Vaginal birth after cesarean (VBAC) is possible, but it depends on several factors like the previous indication, gap between pregnancies, number of previous C-sections, and presence of complications like diabetes or hypertension. The risks, including scar rupture (less than 3%), must be discussed with the healthcare provider. An informed decision is made after weighing the pros and cons.
What are the potential long-term health implications for mothers who deliver via C-section?
C-sections can have long-term implications like adhesions causing pain and discomfort, and a scarred uterus can increase risks in future pregnancies, such as placenta accreta or uterine rupture. However, when indicated, C-sections are life-saving, and the risk of complications is relatively low. The benefits outweigh the risks in high-risk cases.
How common is it for first-time mothers to opt for planned C-sections?
Planned C-sections for non-medical reasons are more common in women who have had previous C-sections, rather than first-time mothers. However, some primies, especially those with subfertility conceptions or IVF, may opt for planned C-sections to avoid risks. But overall, the incidence of primies choosing planned C-sections is relatively low.